Preventive healthcare has always been the gold standard: catching disease before it becomes serious, treating early, enabling better outcomes, and reducing costs. But until recently, there was a gap between what was theoretically possible and what was practical. In 2025, that gap is shrinking fast. With advances in AI, machine learning, and wearables, healthcare is shifting from reactive → proactive. No longer must patients wait for symptoms to become severe. Technology is giving time back.
1. What are AI-Powered Wearables & Remote Monitoring
These are devices and systems that continuously or periodically track health metrics (heart rate, glucose, oxygen saturation, temperature, etc.) and use AI/ML algorithms to analyze the data in real time or near-real time. Remote monitoring means data is sent to healthcare providers (or centralized systems) so interventions can happen outside of hospitals. Key differences vs older devices:
- Devices are smarter: not just collecting raw data but detecting subtle patterns (e.g. irregular heart rhythms). StartUs Insights+1
- Sensors are getting smaller, more accurate, even integrated into fabric or patches. World Wide Digest+2readbeyondmag+2
- Connectivity and cloud/edge computing make it possible to monitor and act on data immediately.
2. Major Trends Driving Adoption
- Continuous Biosensors & Non-Invasive Monitoring: Continuous Glucose Monitors (CGMs) for diabetics, wearable patches, even sensors embedded in clothing or smart fabrics. World Wide Digest+2blip.school+2
- AI & Machine Learning for Signal Processing & Predictive Analytics: Not just measuring, but predicting. For example, AI models that detect risk of heart issues, or flag early onset disease. LinkedIn+2totalmed.com+2
- Remote Patient Monitoring (RPM) Platforms: Systems that aggregate data, alert health providers, reduce hospital re-admissions, help those in rural or underserved areas. totalmed.com+2Forbes+2
- Smart Fabrics / Wearable Tech Fusion: Clothing or patches that are comfortable and stylish, yet function as health trackers. This makes wearables less obtrusive, better suited for long-term monitoring. blip.school+1
- Mental Health & Wellness Tracking: Beyond vitals, wearables are increasingly focused on mood, stress, sleep quality, etc. AI aids in interpreting signals for non-physical health. blip.school+1
3. Top Use Cases
- Chronic Disease Management: Diabetes, hypertension, cardiovascular disease—continuous monitoring helps maintain control, and AI can suggest adjustments or warn of danger.
- Early Detection: For example, devices like AI-powered stethoscopes can detect heart failure, valve disease, or arrhythmias in seconds. The Guardian
- Post-operative Care and Remote Recovery: Monitoring vitals at home, sending alerts if recovery isn’t proceeding well, reducing hospital stay lengths.
- Preventive Health & Wellness: Fitness tracking, sleep monitoring, stress management, early detection of respiratory problems or infections.
- Mental Health Monitoring: Tracking physiological proxies for stress/anxiety; combining with app-based interventions, behavioral prompts.
4. Benefits — for Patients & Health Systems
- Early Detection and Intervention: Catching disease before it worsens increases survival, reduces complications.
- Personalization of Treatment: Data-driven insights create treatment or wellness plans tailored to an individual’s physiology and lifestyle.
- Reduced Costs: Fewer hospitalizations, less emergency care, better chronic disease control.
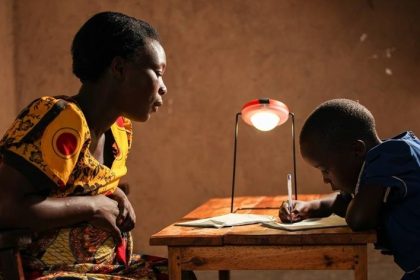
- Better Access / Equity: For those in remote or underserved regions, remote monitoring means less travel, more consistent care.
- Less Strain on Healthcare Workers: Automation of routine monitoring & alerts means clinicians spend more time on complex cases.
5. Challenges & Risks
- Data Privacy & Security: Sensitive health data is being transmitted; risk of breaches, misuse of data.
- Accuracy & False Positives / Negatives: Sensors and algorithms are not perfect; false alarms can cause anxiety or unnecessary interventions.
- Regulatory & Compliance Issues: Medical regulation in many countries lags behind technological innovation. Ensuring safety, efficacy, and approval is nontrivial.
- Equity & Access: Devices cost money; infrastructure like stable internet/telecom is needed; digital literacy matters. If not addressed, can worsen health disparities.
- User Compliance: Wearables must be comfortable, battery-efficient, reliable. If they are inconvenient, people will stop using them.
6. Real-World Examples & Case Studies
- An AI stethoscope developed in London (by Imperial College etc.) can detect heart failure, valve disease, and irregular rhythms in “just 15 seconds.” The Guardian
- Increasing deployment of AI-enabled cancer screening devices (breast, cervical, etc.) by governments in India to improve early detection. The Times of India+1
- Widespread use of CGMs and wearable ECGs to monitor diabetic or cardiac patients remotely. Forbes+1
7. What to Expect Next: The Road Ahead
- Generative AI & Decision Support: More tools will assist clinicians, summarizing data, suggesting diagnostics, helping planning. LinkedIn+1
- Non-Invasive, Multi-Modal Sensors: Sensors that read biomarkers non-invasively (e.g. via skin, sweat), combining different signals (heart, respiration, movement, biochemical).
- Stronger Focus on Ethics, Bias & Regulatory Frameworks: Addressing bias in training data; ensuring marginalized populations are included; developing laws/regulation around AI in health. arXiv+1
- Edge Computing & On-Device AI: To reduce latency, preserve privacy, allow operation even without continuous internet.
- Integration with Telehealth & Digital Therapeutics: Wearables becoming key components in broader care pathways.
AI-powered wearables and remote patient monitoring are not just futuristic ideas anymore—they’re here, and shaping preventive healthcare in real ways. As sensors get smarter, AI gets more capable, and access improves, this tech promises earlier detection, more personalized care, lower costs, and healthier populations. But it’s essential to address privacy, accuracy, equity, and regulatory oversight so the promise is lived by all.
If you’re a patient: consider trying out a validated wearable, discuss remote monitoring with your health provider. If you’re a provider or policy-maker: invest in infrastructure, regulation, and programs that make this tech accessible.